Impact of Obesity on Knee Replacement Surgery and Recovery
September 30, 2025Introduction
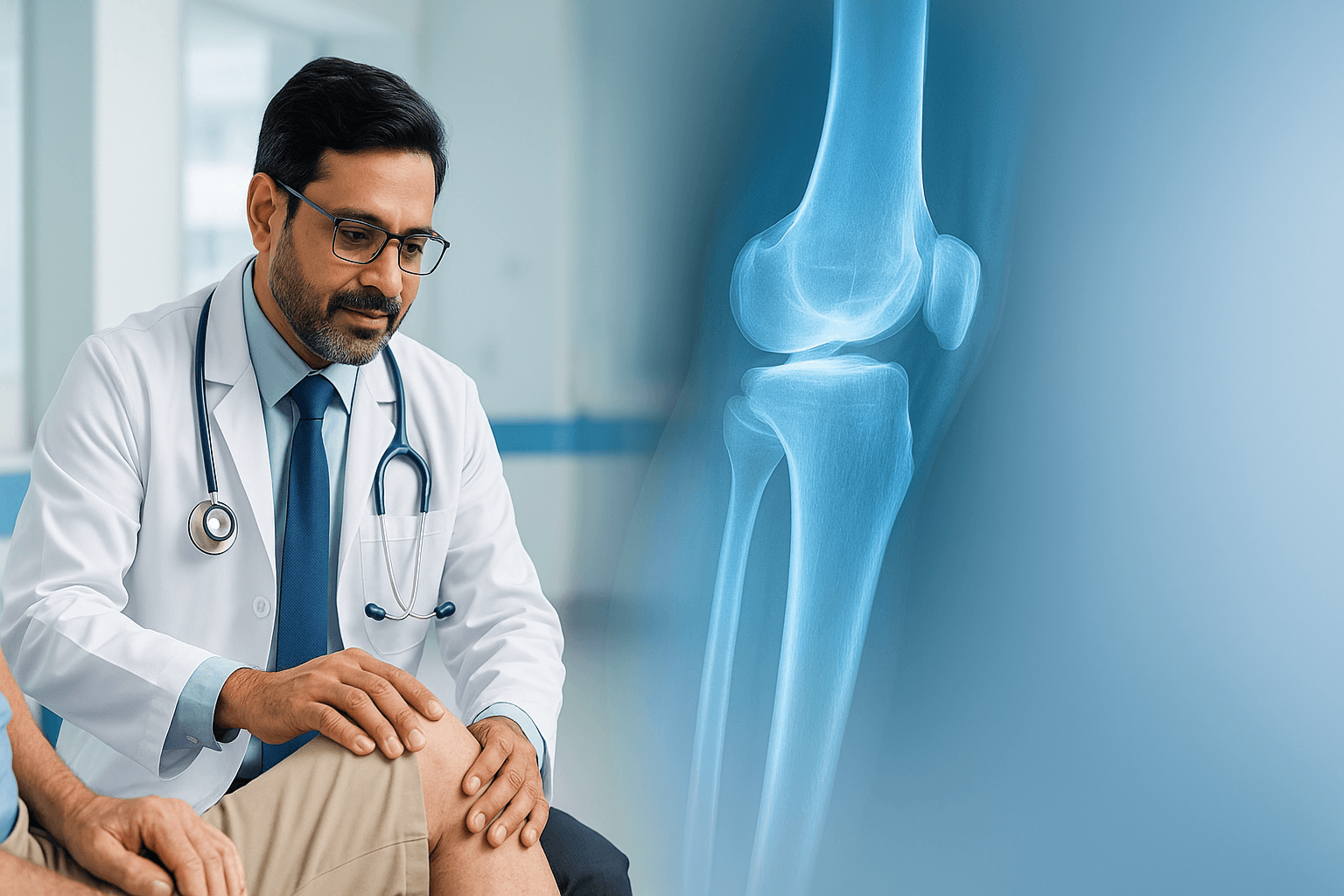
Knee replacement (arthroplasty) is a life-changing surgery for many patients suffering from severe arthritis, joint degeneration, or injury. However, the outcome and recovery of a knee replacement surgery are influenced by many patient factors — one of the the most important being obesity. In this blog, we will explore how obesity affects knee replacement surgery and recovery, what special precautions are needed, and how a top surgeon can mitigate risks. We’ll also introduce Dr Deepak Mishra, widely regarded as one of the best knee replacement & orthopedic specialists in Faridabad, and how his approach helps patients with higher body mass index (BMI).
What is obesity and why does it matter for joints?
- Definition: Obesity is typically defined by Body Mass Index (BMI). A BMI of 30 or more is considered obese (this threshold may be lower in some Asian populations).
- Mechanical load: Extra body weight increases the mechanical load on weight-bearing joints like the knees. Every additional kilogram of body weight translates into several kilograms of pressure across the knee joint during walking, standing, stair-climbing, etc.
- Joint wear & tear: Over time, the increased load accelerates cartilage wear, causes inflammation, meniscus degeneration, and structural changes in bone alignment. Many patients with obesity show earlier onset and more severe knee osteoarthritis.
- Systemic inflammation: Obesity is associated with low-grade systemic inflammation, which may degrade cartilage and slow healing after surgery. Adipose tissue also secretes inflammatory mediators.
Because of these mechanisms, obesity is a major risk factor for needing knee replacement surgery earlier than otherwise, and it influences surgical planning and outcomes.
How obesity affects knee replacement surgery
1. Surgical challenges & intraoperative risks
- Exposure difficulties: Excess fat in soft tissues may make it harder for the surgeon to access the joint, requiring deeper dissections and more soft-tissue retraction.
- Longer operative time: Difficult exposure often increases operating time, which in turn raises risk of infection, bleeding, and anesthesia-related complications.
- Bleeding and wound issues: Soft tissues may not heal as well, and excess adipose tissue may impair wound perfusion, increasing risk of wound dehiscence or superficial infection.
- Instrumentation fit & alignment: Obese patients may present anatomical differences in bone geometry (e.g. more varus/valgus alignment shifts) or challenges in positioning. Ensuring precise implant alignment is critical; misalignment leads to accelerated wear or failure.
- Need for stronger implants: In some cases, a surgeon may opt for implants with improved fixation (e.g. stem extensions, more robust fixation) to handle greater load.
Because of these challenges, knee replacement in obese patients demands extra planning, surgical skill, and care.
2. Increased complications & risk factors
Patients with obesity tend to have higher rates of:
- Infection: Both superficial (skin, subcutaneous) and deeper wound infections due to sluggish wound healing and reduced perfusion.
- Thromboembolic events (DVT / PE): Obesity is a known risk factor for thrombosis.
- Delayed wound healing: Poor microcirculation in fatty tissues may slow the closure and healing of surgical incisions.
- Loosening / implant failure: Excess load may stress the bone–implant interface, risking micro-motion or loosening over time.
- Perioperative pulmonary / cardiovascular risks: Obesity is often associated with comorbidities (hypertension, diabetes, sleep apnea, cardiovascular disease) that increase anesthesia risk, cardiopulmonary events, and complications.
- Lower functional outcome / slower recovery: Some studies show that patients with obesity have a slower or somewhat lesser functional gain postoperatively, particularly in early months.
Thus, the surgeon must anticipate and mitigate these risks.
Strategies to improve outcomes in obese knee replacement patients
Pre-operative optimization
- Weight loss
- Even modest weight reduction (5–10% of body weight) can reduce joint stress and improve surgical outcomes.
- Nutritious low-calorie diet, supervised exercise, and possibly medically guided weight-loss programs are beneficial.
- Medical optimization
- Control of comorbidities: Diabetes, hypertension, obstructive sleep apnea, cardiac disease.
- Nutritional status: Correct anemia, ensure protein intake, vitamin levels, etc.
- Prehabilitation / physiotherapy
- Strengthening surrounding muscles (quadriceps, hamstrings, hip muscles) helps joint stability.
- Range-of-motion drills to maintain mobility before surgery.
- Detailed surgical planning
- Use advanced imaging (CT, MRI) to understand bone geometry.
- Plan implant size, alignment strategies, soft-tissue balancing, and contingencies for difficult exposure.
Intraoperative best practices
- Use minimally invasive or careful soft-tissue–sparing approaches when feasible.
- Meticulous hemostasis (control bleeding) to reduce hematoma.
- Use of prophylactic antibiotics (broad spectrum) and sterile techniques to reduce infection risk.
- Careful soft-tissue handling to preserve blood supply to skin and tissues.
- Precise implant alignment and balancing to distribute loads optimally.
- Considering robotic or navigation-assisted surgery (if available) to improve precision (especially helpful in challenging anatomies).
Postoperative & rehabilitation strategies
- Wound care protocols: Use of advanced dressings, suction drains, delayed mobilization if wound risk, close monitoring.
- Thromboprophylaxis: Extended anticoagulation as per risk (given obesity).
- Physical therapy: Early mobilization, progressive weight-bearing, muscle strengthening, gait training.
- Nutrition & protein supplementation: Support healing with adequate protein, micronutrients.
- Close follow-up: Early detection of complications (infection, wound issues, DVT) enables prompt intervention.
With these strategies, many obese patients can achieve good outcomes, albeit with more vigilance.
Evidence from studies: What does research say?
- Many observational studies document higher complication rates (wound problems, infections, reoperations) in obese vs. non-obese knee replacement patients.
- However, long-term functional gains (pain relief, mobility) may still be substantial even in obese patients, provided surgery is well executed and postoperative care is optimal.
- Some studies suggest that while early functional recovery might lag, at 1–2 years the difference in functional scores may narrow.
- Use of navigation / robotic-assisted surgery has been proposed to reduce alignment errors and improve implant positioning especially in challenging anatomies — thus mitigating some of the excess risk in obese patients.
Why choosing the right surgeon matters — Introducing Dr Deepak Mishra
When dealing with the additional complexities of knee replacement in obese patients, the experience, skill, and infrastructure of the operating surgeon and center make a big difference.
Dr Deepak Mishra is widely recognized as a leading orthopedic and joint replacement surgeon in Faridabad / Delhi NCR.
Here’s what sets him apart:
- Experience & specialization: He has over 26 years of experience in joint replacement and arthroscopic surgery.
- Robotic & computer-navigated surgery: He works with advanced robotic systems (e.g. MISSO robotic systems) to improve accuracy in knee replacement, which is especially beneficial in anatomically challenging or obese patients.
- Comprehensive approach: Dr Mishra’s practice emphasizes preoperative planning, optimization, post-operative rehabilitation, and personalized patient care.
- Leadership role: He is the Director & Head of the Orthopaedics & Joint Replacement unit at Asian Hospital, Faridabad.
- Reputation & recognition: Local listings and hospital websites refer to him as among the best orthopedic doctors in Faridabad, especially for knee and hip replacement.
Because of this blend of technical skill, infrastructure, and experience, Dr Deepak Mishra is often a top choice for patients with higher risk profiles — such as obese individuals — who require knee replacement surgery.
Key takeaways & advice for patients with obesity
- Don’t postpone evaluation
- If you are struggling with knee pain / arthritis and are obese, consult an experienced knee replacement surgeon early. Delaying may lead to further joint damage and worse outcomes.
- Work on weight reduction before surgery
- Even modest weight loss can make surgery safer and recovery easier.
- Choose a surgeon with experience in high-risk patients
- A surgeon who has handled obese patients before, uses navigation/robotics, and understands soft-tissue challenges will offer better outcomes.
- Follow through with rehabilitation & care
- Recovery is more demanding in obese patients — strict adherence to physiotherapy, wound care, follow-up, and lifestyle change is essential.
- Set realistic expectations, but not pessimistic ones
- Yes, some risks are higher — but many obese patients eventually achieve significant pain relief, improved mobility, and better quality of life if things go well.
Recent Blogs
-
 ACL Tears in Athletes: Symptoms, Treatment Options & Recovery
ACL Tears in Athletes: Symptoms, Treatment Options & Recovery- 19, November 2025
-
 Sports Injuries That Often Lead to Knee Replacement
Sports Injuries That Often Lead to Knee Replacement- 19, November 2025
-
 Orthopedic Care for Elderly Patients — A Complete Guide
Orthopedic Care for Elderly Patients — A Complete Guide- 12, November 2025
-
 How Long Do Knee Implants Last? (10–20 Year Longevity Guide)
How Long Do Knee Implants Last? (10–20 Year Longevity Guide)- 12, November 2025
-
 Importance of Early Diagnosis in Bone and Joint Problems
Importance of Early Diagnosis in Bone and Joint Problems- 28, October 2025
-
 Best Treatment Options for Sports Injuries
Best Treatment Options for Sports Injuries- 28, October 2025
-
 The Difference Between ACL Tear, Sprain, and Rupture
The Difference Between ACL Tear, Sprain, and Rupture- 16, October 2025
-
 Post-ACL Surgery Do’s and Don’ts
Post-ACL Surgery Do’s and Don’ts- 16, October 2025
-
 Early Signs You Might Have an ACL Injury (and When to See a Doctor)
Early Signs You Might Have an ACL Injury (and When to See a Doctor)- 16, October 2025
-
 Does Insurance Cover Robotic Knee Replacement Surgery?
Does Insurance Cover Robotic Knee Replacement Surgery?- 6, October 2025
-
 When Can You Return to Sports After Robotic Knee Replacement?
When Can You Return to Sports After Robotic Knee Replacement?- 6, October 2025
-
 Impact of Obesity on Knee Replacement Surgery and Recovery
Impact of Obesity on Knee Replacement Surgery and Recovery- 30, September 2025
-
 Early vs. Delayed Knee Replacement: Which Is Better?
Early vs. Delayed Knee Replacement: Which Is Better?- 30, September 2025
-
 How Durable Are Knee Implants? A Complete Guide
How Durable Are Knee Implants? A Complete Guide- 24, September 2025
-
 Can You Play Sports After Knee Replacement Surgery?
Can You Play Sports After Knee Replacement Surgery?- 24, September 2025
-
 Key Benefits of Revision Hip Replacement You Should Know
Key Benefits of Revision Hip Replacement You Should Know- 15, September 2025
-
 Revision Hip Replacement vs. Primary Hip Replacement: Key Differences
Revision Hip Replacement vs. Primary Hip Replacement: Key Differences- 15, September 2025
-

-
 Total Knee Replacement Complications: What You Need to Know
Total Knee Replacement Complications: What You Need to Know- 5, September 2025
-
 Can You Play Sports After Hip Replacement Surgery?
Can You Play Sports After Hip Replacement Surgery?- 26, August 2025
-
 Preparing for Knee Replacement: Do’s and Don’ts Before Surgery
Preparing for Knee Replacement: Do’s and Don’ts Before Surgery- 26, August 2025
-

-
 What to Know About Knee Replacement Revision Surgery
What to Know About Knee Replacement Revision Surgery- 18, August 2025
-
 Cost of Hip Replacement in India – What Patients Should Know
Cost of Hip Replacement in India – What Patients Should Know- 11, August 2025
-

-
 Who Is the Best Orthopedic Doctor for Sports Injuries?
Who Is the Best Orthopedic Doctor for Sports Injuries?- 27, July 2025
-
 Success Rate of Robotic Knee Replacement in India
Success Rate of Robotic Knee Replacement in India- 27, July 2025
-
 Why Surgeons Are Switching to Robotic Knee Replacements
Why Surgeons Are Switching to Robotic Knee Replacements- 15, July 2025
-
 Do’s and Don’ts After Knee Replacement Surgery
Do’s and Don’ts After Knee Replacement Surgery- 15, July 2025
-
 Best Robotic Knee Replacement in India
Best Robotic Knee Replacement in India- 7, July 2025
-
 Affordable Robotic Knee Replacement in India
Affordable Robotic Knee Replacement in India- 7, July 2025
-

-

-

-

-

-

-

-
 Orthopedic Meaning, Definition, Types, and More
Orthopedic Meaning, Definition, Types, and More- 6, June 2025
-
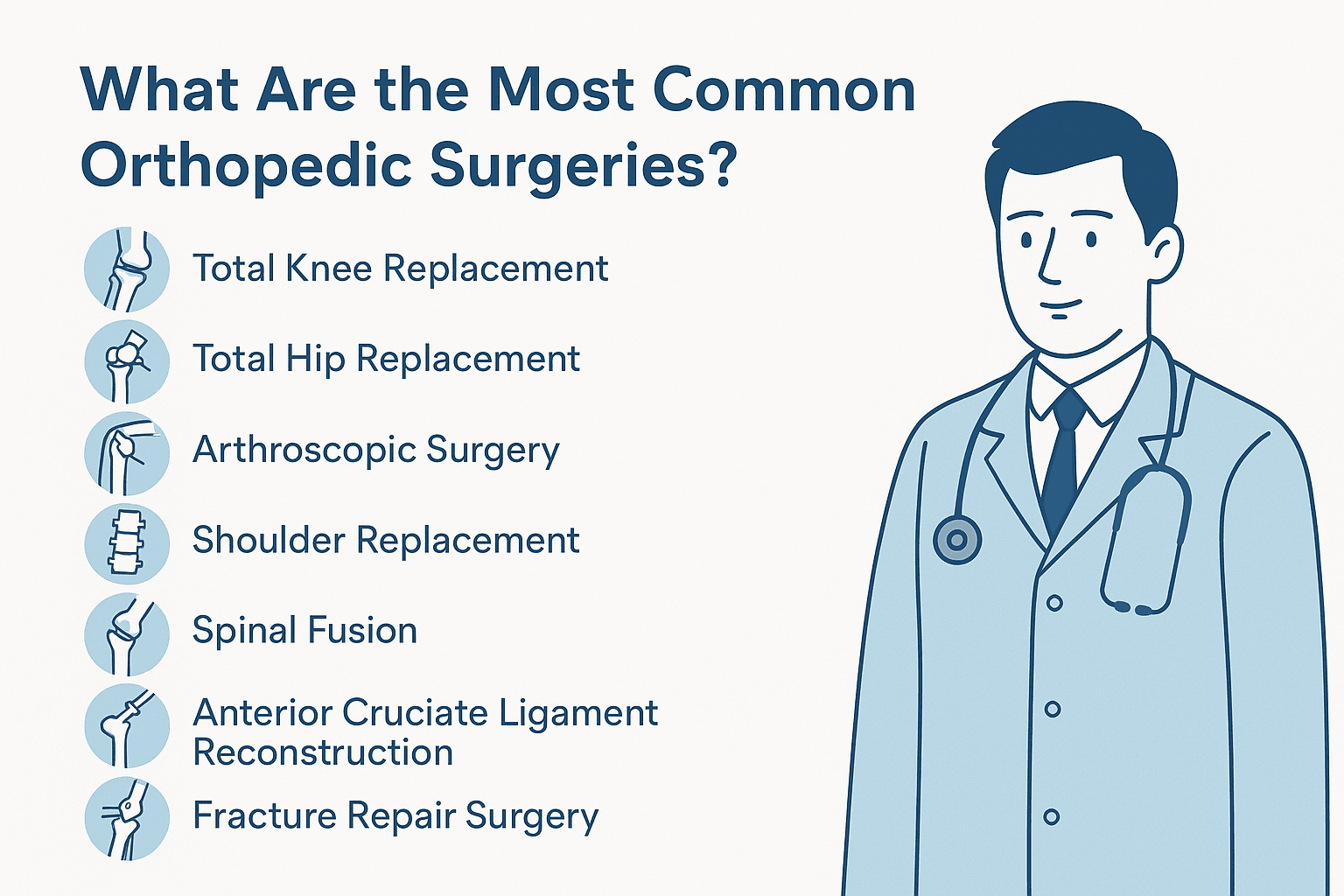
 What Are the Most Common Orthopedic Surgeries?
What Are the Most Common Orthopedic Surgeries?- 24, May 2025
-
 What Does an Orthopedic Doctor Do?
What Does an Orthopedic Doctor Do?- 24, May 2025
-

-

-

-
 Best Orthopedic Doctor for Knee Pain in Faridabad
Best Orthopedic Doctor for Knee Pain in Faridabad- 12, May 2025
-
 How to Prevent Knee Pain with Orthopedic Expert Tips
How to Prevent Knee Pain with Orthopedic Expert Tips- 29, April 2025
-

-
 Best Orthopedic Treatment in Faridabad: What You Should Know
Best Orthopedic Treatment in Faridabad: What You Should Know- 29, April 2025
-

-

-
 Best Knee Replacement Surgeon in Mathura
Best Knee Replacement Surgeon in Mathura- 14, April 2025
-
 Best Knee Replacement Surgeon in Hodal
Best Knee Replacement Surgeon in Hodal- 14, April 2025
-
 Best Knee Replacement Surgeon in Palwal
Best Knee Replacement Surgeon in Palwal- 14, April 2025
-

-

-

-
 Benefits of Minimally Invasive Knee Surgery
Benefits of Minimally Invasive Knee Surgery- 24, March 2025
-
 Types of Knee Implants
Types of Knee Implants- 17, March 2025
-
 Best knee Replacement Surgeon in India
Best knee Replacement Surgeon in India- 17, March 2025
-

-
 How to Recover Quickly After Knee Replacement Surgery
How to Recover Quickly After Knee Replacement Surgery- 10, March 2025
-

-

-

-
 Minimally Invasive Arthroplasty: Benefits and Recovery Advantages
Minimally Invasive Arthroplasty: Benefits and Recovery Advantages- 24, February 2025
-
 Common Mistakes to Avoid After Joint Replacement Surgery
Common Mistakes to Avoid After Joint Replacement Surgery- 24, February 2025
-
 Choosing the Right Hip Replacement Surgeon: A Comprehensive Guide
Choosing the Right Hip Replacement Surgeon: A Comprehensive Guide- 17, February 2025
-
 Restoring Mobility: The Role of Knee Replacement Doctors
Restoring Mobility: The Role of Knee Replacement Doctors- 17, February 2025
-
 Orthopedic Trauma Care for Athletes
Orthopedic Trauma Care for Athletes- 6, February 2025
-
 Best Doctor for ACL Tear Treatment
Best Doctor for ACL Tear Treatment- 6, February 2025
-
 Best Sports Medicine Doctor for Knee Injuries
Best Sports Medicine Doctor for Knee Injuries- 6, February 2025
-
 Orthopedic Surgeons: 7 Things You Need to Know
Orthopedic Surgeons: 7 Things You Need to Know- 27, January 2025
-
 Best Joint Replacement Surgeon in Greater Faridabad
Best Joint Replacement Surgeon in Greater Faridabad- 27, January 2025
-
 Best Knee Replacement Surgeon in Palwal
Best Knee Replacement Surgeon in Palwal- 20, January 2025
-
 Best Knee Replacement Surgeon in South Delhi
Best Knee Replacement Surgeon in South Delhi- 20, January 2025
-
 Signs You May Need a Knee Replacement: Insights from a Surgeon
Signs You May Need a Knee Replacement: Insights from a Surgeon- 13, January 2025
-
 Restoring Mobility: The Role of Knee Replacement Doctor
Restoring Mobility: The Role of Knee Replacement Doctor- 13, January 2025
-
 Robotic Knee Replacement Surgery in Delhi
Robotic Knee Replacement Surgery in Delhi- 30, December 2024
-
 Robotic Orthopedic Surgery: Revolutionizing Joint Replacement and Repair
Robotic Orthopedic Surgery: Revolutionizing Joint Replacement and Repair- 30, December 2024
-
 Robotic Knee Replacement vs. Traditional Surgery: A Comparative Guide
Robotic Knee Replacement vs. Traditional Surgery: A Comparative Guide- 23, December 2024
-
 How to Make Joints Stronger: A Comprehensive Guide
How to Make Joints Stronger: A Comprehensive Guide- 23, December 2024
-
 Common Knee Conditions and How a Knee Surgeon Can Help
Common Knee Conditions and How a Knee Surgeon Can Help- 16, December 2024
-

-

-
 Orthopedic Surgeons: 7 Things You Need to Know
Orthopedic Surgeons: 7 Things You Need to Know- 6, December 2024
-
 Top 5 Mistakes After Knee Replacement
Top 5 Mistakes After Knee Replacement- 25, November 2024
-
 Advantages and Disadvantages of Robotic Knee Replacement
Advantages and Disadvantages of Robotic Knee Replacement- 25, November 2024
-
 When to See an Orthopedic Specialist: Recognizing Early Signs
When to See an Orthopedic Specialist: Recognizing Early Signs- 15, November 2024
-
 Benefits of Robotic-Assisted Knee Replacement Surgery
Benefits of Robotic-Assisted Knee Replacement Surgery- 15, November 2024
-
 Knee Replacement Surgery Cost
Knee Replacement Surgery Cost- 8, November 2024
-
 Best Robotic Knee Replacement Surgeon in Faridabad
Best Robotic Knee Replacement Surgeon in Faridabad- 8, November 2024
-

-
 Knee Replacement Surgery: Types, Benefits, and Recovery Timeline
Knee Replacement Surgery: Types, Benefits, and Recovery Timeline- 28, October 2024
-
 What is Osteoporosis? Symptoms, Causes, and Prevention
What is Osteoporosis? Symptoms, Causes, and Prevention- 21, October 2024
-
 Signs It’s Time for a Knee Replacement: When to Consult a Surgeon
Signs It’s Time for a Knee Replacement: When to Consult a Surgeon- 18, October 2024
-
 Understanding Different Types of Arthritis: Symptoms and Causes
Understanding Different Types of Arthritis: Symptoms and Causes- 11, October 2024
-
 Taking Care After Knee Replacement Surgery
Taking Care After Knee Replacement Surgery- 15, December 2022
-
 Amazing Ways to Get Relief from Arthritis Pain Naturally
Amazing Ways to Get Relief from Arthritis Pain Naturally- 2, December 2022
-

-
 How Does Fat Affect Arthritis?
How Does Fat Affect Arthritis?- 4, November 2022