Early vs. Delayed Knee Replacement: Which Is Better?
September 30, 2025Knee replacement (also called knee arthroplasty) is a major decision for patients suffering from debilitating knee pain, stiffness, or reduced mobility—typically due to arthritis, injury, or degeneration of the joint. One of the ongoing debates in orthopedic care is when to opt for knee replacement: should one proceed early or wait until symptoms worsen? In this article, we’ll examine the pros and cons of early vs. delayed knee replacement, help readers weigh the options, and explain how to decide the optimal timing along with considerations in the Indian context.
Understanding Knee Replacement
Before diving into timing, let’s briefly recap what knee replacement entails:
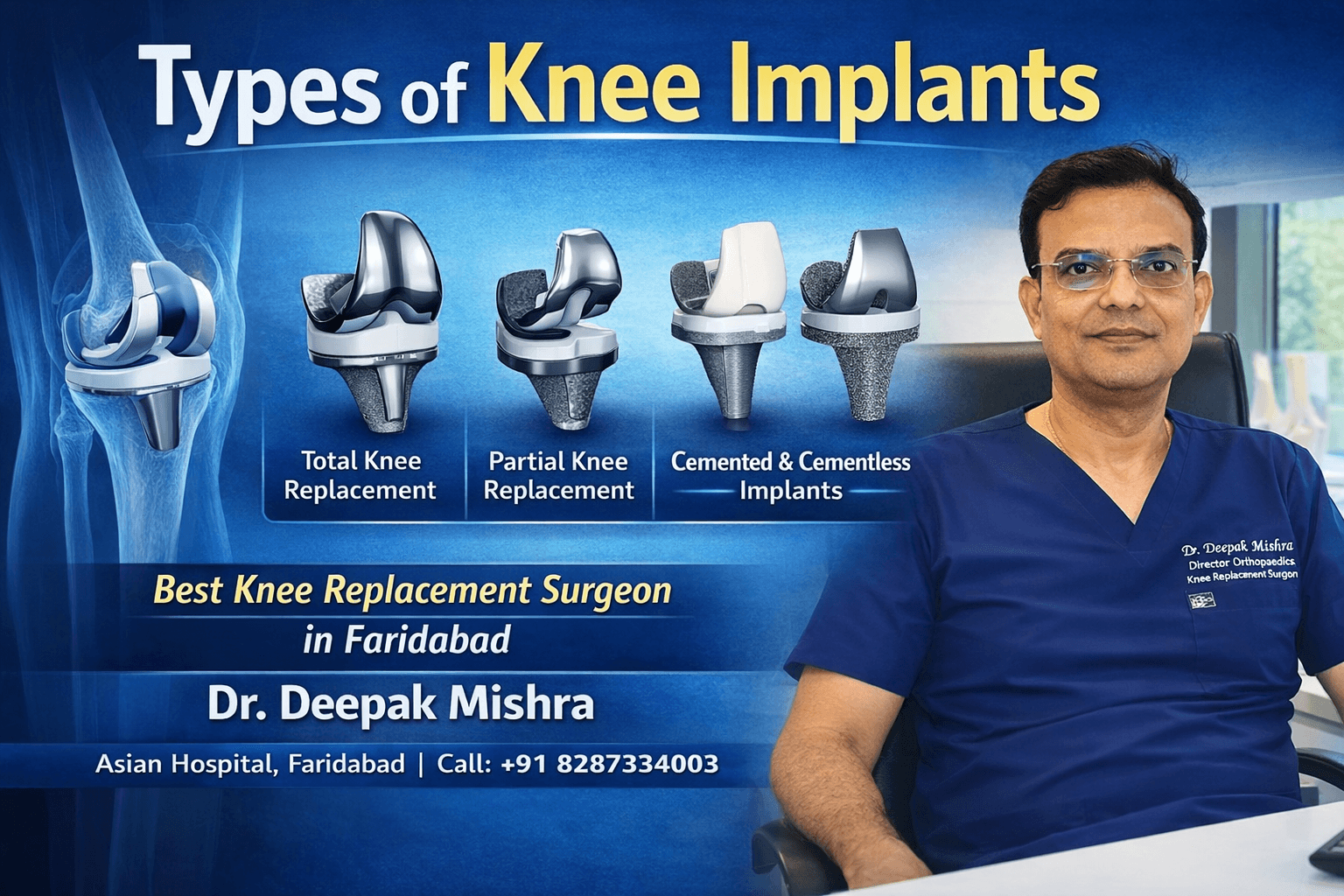
- In total knee replacement (TKR), damaged joint surfaces (femur, tibia, possibly patella) are removed and replaced with prosthetic components.
- In some patients, partial (unicompartmental) knee replacement is an option if only one compartment of the knee is severely affected.
- Modern advancements include robotic‐assisted knee replacement (or computer-assisted navigation) to improve alignment, precision, and potentially outcomes.
- Postoperative rehabilitation (physio, muscle strengthening, gait training) is critical to regain function.
What Does “Early” and “Delayed” Mean?
- Early knee replacement generally refers to performing surgery before severe deformity, joint collapse, or extensive bone loss occurs—and while the patient still has some remaining joint function and muscle strength.
- Delayed (or late) knee replacement means postponing the surgery until the disease or symptoms are advanced, when non-surgical treatments (medications, injections, physiotherapy, braces) no longer provide relief.
There is no universally fixed cut-off, but the decision is individualized based on pain severity, quality of life, functional limitation, radiographic status, and patient factors (age, comorbidities, activity level).
Pros & Cons: Early Knee Replacement
Benefits of Early Replacement
- Better functional outcomes
When surgery is done before the knee joint is severely deformed or muscle wasting has set in, patients often achieve better restoration of mobility, range of motion, and strength. - Less compensatory strain on other joints
With a painful knee, patients may favor the other leg, hips or spine, leading to secondary problems. Early correction stops these maladaptive patterns. - Improved quality of life sooner
Patients suffering from moderate pain or reduced activity can return to normal life earlier, rather than prolong suffering. - Simpler surgery, less bone loss
In earlier stages, bone quality tends to be better, deformities are milder, and soft tissue contractures are fewer—making the surgery technically easier. - Lower risk of progressive damage
Delaying might allow further deterioration of bone, ligaments, or surrounding structures, making later surgery more complex or less effective.
Potential Drawbacks or Considerations
- Longevity of implant
If one is younger, the prosthetic may wear out in one’s lifetime (though modern implants now last 15-25 years in many cases). Early surgery might lead to revision later. - Surgical risk earlier than necessary
Some patients may manage adequately with conservative measures for a while; operating “too early” might expose them to surgical risk prematurely. - Cost and resource considerations
In resource-limited settings, prioritizing patients with more advanced disease might sometimes be the practical choice. - Psychological readiness
Some patients are hesitant to commit to a major surgery when they still have some function.
Pros & Cons: Delayed (Later) Replacement
Benefits of Delayed Replacement
- Maximizing conservative therapy
One can attempt to exhaust nonoperative modalities (physio, injections, weight loss, bracing) before resorting to surgery. - Delay wearing out the implant
Especially in younger patients, delaying surgery may delay the time when a revision is needed. - Avoiding surgery when not strictly needed
Some patients may maintain acceptable function for years; delaying avoids surgical risk until absolutely necessary.
Risks & Disadvantages of Delayed Replacement
- Worsening deformity and bone loss
More advanced disease leads to more complex anatomy (bone defects, ligament contractures, malalignment), increasing surgical difficulty and risk. - Muscle atrophy & poor soft-tissue condition
Long periods of pain and limited use lead to wasting of the quadriceps, hamstrings, and other supporting muscles, making rehabilitation harder. - Lower functional gains
Patients who wait too long may not recover as fully, even after surgery, compared to those who operated earlier. - Higher risk of comorbid complications
Delay may allow comorbidities (e.g. cardiovascular issues, diabetes, obesity) to worsen, increasing surgical risk. - Diminished quality of life for longer
Prolonged pain, immobility, disability, dependency on medicines, and negative psychosocial impact.
What Does the Evidence Say?
Medical literature suggests a balance is needed. Some studies show that patients who opt for knee replacement when symptoms become moderate (rather than severe), often achieve similar (or better) outcomes with fewer complications and better functional recovery. Waiting until the disease is very advanced might reduce the magnitude of benefit.
However, each patient is unique. Timing decisions should factor:
- Symptom severity and frequency
- Impact on daily living
- Radiographic progression
- Patient age, comorbidities, and expectations
- Bone quality, deformities, and surgical complexity
Early vs. Delayed: Which Is Better? (Contextual Factors)
The “better” choice depends on individual circumstances. Here’s how to think about it:
| Scenario | Early Replacement Favored | Delayed Replacement Favored |
|---|---|---|
| Middle-aged patient with moderate pain interfering with daily life, despite therapy | Early | — |
| Elderly patient with slow progression, tolerable symptoms | — | Delayed (if conservative measures work) |
| Evidence of rapid degeneration, joint collapse, bone defects | Early (to prevent worsening) | — |
| Young patient (50s) with moderate symptoms | Balance carefully (risk vs benefit) | Possible delay if function acceptable |
| Comorbidities increasing surgical risk | Delay until optimized | — |
So, in many patients, earlier intervention (before severe joint destruction) offers better restoration of function and quality of life, especially when nonoperative treatments are failing.
Robotic & Navigation-Assisted Knee Replacement: Does Timing Matter?
Robotic-assisted and computer-navigated systems offer:
- Higher precision in bone cuts and alignment
- Optimized implant positioning
- Less soft-tissue trauma
- Potential for faster recovery
Because these systems rely on planning based on existing anatomy, earlier intervention (when deformities are not extreme) can maximize the benefit of robotic precision. When deformities are severe, robotic systems may still help but with extra challenges.
Thus, early surgery may allow surgeons to fully exploit robotic advantages and achieve optimal alignment and stability, promoting long-term success.
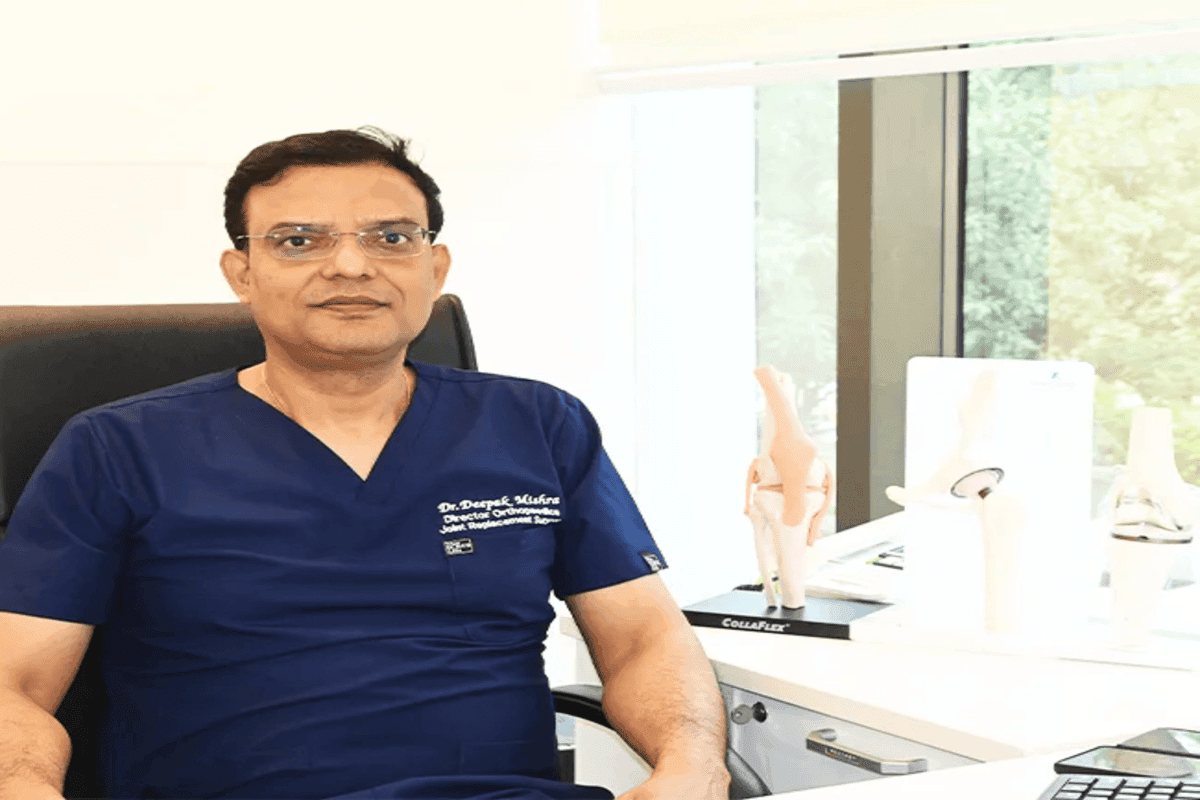
Why Choosing the Right Surgeon Matters — Enter Dr. Deepak Mishra
If you are considering knee replacement in Faridabad or nearby, one name stands out: Dr. Deepak Mishra. He has been widely praised as the best knee replacement surgeon in Faridabad and the top orthopedic doctor in Faridabad
Key Credentials & Strengths
- Experience & Expertise: Over 25–26 years of practice in joint replacement, arthroscopy, hip & knee surgery.
- Leadership Role: Director & Head of Orthopedics / Joint Replacement at Asian Hospital, Faridabad.
- Recognition in Region: Known locally as a top orthopedic surgeon in Delhi NCR and Faridabad in joint replacement & knee surgery.
- Holistic Patient Approach: He is reputed for personalized care, detailed preoperative evaluation, surgical precision, and strong postoperative rehabilitation support.
When determining timing (early vs. delayed) for knee replacement, expertise and judgment are crucial. A surgeon like Dr. Mishra can help assess the optimal window for surgery, tailoring the timing to patient anatomy, disease progression, expectations, and comorbidities.
Practical Decision Guide: Early vs. Delayed
Here’s a simplified decision path you can share in your blog or clinic materials:
- Begin with conservative care
Try physical therapy, weight reduction, anti-inflammatories, pain management, injections (if applicable). - Monitor progression
Use periodic imaging (X-rays, MRI) to assess joint degeneration, alignment, bone loss. - Assess impact on life
If pain and stiffness begin to interfere with daily tasks, mobility, sleep, mental health, quality of life—not just occasional discomfort. - Check surgical fitness
Manage comorbidities (diabetes, heart disease, obesity) to reduce surgical risk when time comes. - Consult a specialist early
Don’t wait until you’re severely limited—consult with an experienced knee replacement surgeon like Dr. Mishra early to evaluate timing, even if surgery is not immediate. - Plan for optimal timing
If the patient is primed (bone quality, muscle strength, low comorbidity risk), early procedure may yield best long-term outcomes. - Use advanced techniques
If the surgeon offers robotic or navigated knee replacement, earlier surgery with less deformity may optimize results.
Case Scenarios (Illustrative Examples)
- Case 1: A 60-year-old woman with moderate osteoarthritis, pain during walking > 2 years, tried conservative care but still restricted in daily chores. She has no major comorbidities. Early knee replacement may allow her to regain independence before further joint destruction.
- Case 2: A 70-year-old man with slowly worsening knee pain that is manageable, significant cardiac issues, and mild arthritis changes. He may benefit from delaying surgery until symptoms worsen, while optimizing medical status.
- Case 3: A 55-year-old with rapid joint deterioration (bone loss, deformity) on imaging and high pain despite therapy. Delaying may worsen surgical complexity—early replacement might be optimal.
These scenarios emphasize that there’s no “one size fits all.” The best strategy is timely intervention, based on individualized evaluation by an expert surgeon.
Patient Tips: How to Prepare & What to Ask
- Keep a pain–function diary: track when pain is worst, how it limits life.
- Get serial imaging (X-rays, MRI) to document progression.
- Ask your surgeon:
- Am I an early or delayed candidate?
- Given my age, anatomy, and disease stage, when is ideal timing?
- Do you use robotic / navigated systems?
- What are likely outcomes if I wait vs operate now?
- What is your experience (number of cases, results)?
- Strengthen muscles via physiotherapy pre-habilitation (to ease recovery later).
- Control general health: weight, diabetes, blood pressure—all matter for surgery success.
Key Takeaways & Recommendations
- Early knee replacement can provide superior functional outcomes, prevent secondary joint strain, and allow smoother surgery and rehab—but it must be balanced against implant longevity, patient age, and readiness.
- Delayed replacement has its place, especially when symptoms are tolerable and conservative therapy is still effective.
- The optimal time for surgery is when symptoms meaningfully affect life and further delay risks worsening outcomes—but before severe joint destruction sets in.
- The experience and judgment of the surgeon are critical—choosing a highly skilled surgeon who can assess timing wisely is essential.
- In Faridabad / NCR, Dr. Deepak Mishra is a name many trust as the top knee replacement surgeon and orthopedic specialist, with decades of experience, excellence in joint replacement, and patient-centered care.
Recent Blogs
-
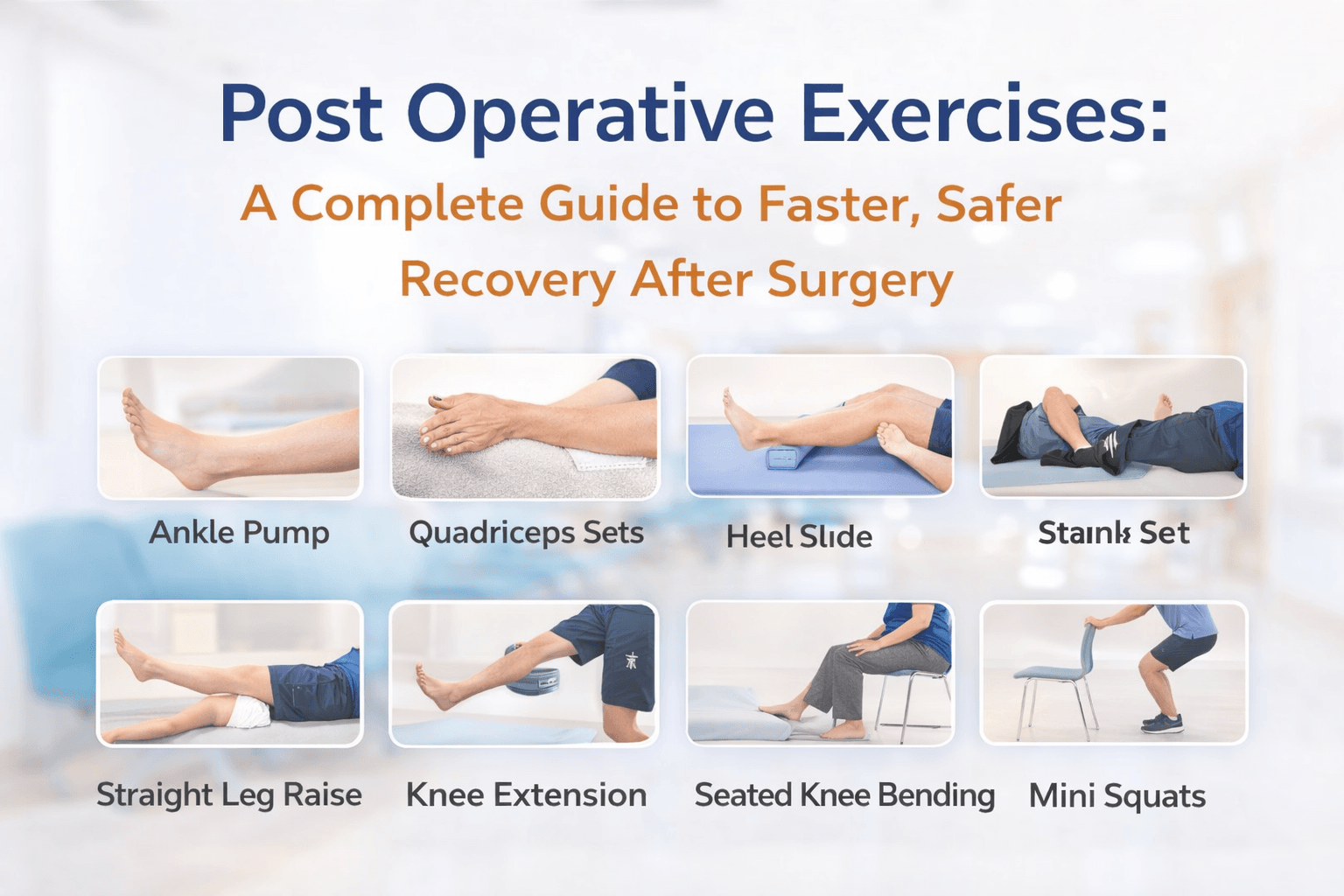
 Post Operative Exercises
Post Operative Exercises- 1, March 2026
-
 After ACL Surgery When Can I Walk?
After ACL Surgery When Can I Walk?- 1, March 2026
-
 What Happens If Knee Arthritis Is Left Untreated?
What Happens If Knee Arthritis Is Left Untreated?- 21, February 2026
-
 Can Knee Replacement Fail? Causes, Signs & Prevention
Can Knee Replacement Fail? Causes, Signs & Prevention- 21, February 2026
-
 Who Is Not Suitable for Knee Replacement Surgery?
Who Is Not Suitable for Knee Replacement Surgery?- 12, February 2026
-
 Best Meniscus Injury Surgeon in Faridabad
Best Meniscus Injury Surgeon in Faridabad- 9, February 2026
-
 How Obesity Affects Knee Health & When to Consider Knee Replacement
How Obesity Affects Knee Health & When to Consider Knee Replacement- 6, February 2026
-
 Knee Pain After Sitting for Long Hours – What to Do
Knee Pain After Sitting for Long Hours – What to Do- 3, February 2026
-
 Most Common Sports Injuries and How to Prevent Them
Most Common Sports Injuries and How to Prevent Them- 26, January 2026
-
 Walking, Stairs & Daily Activities After Knee Replacement
Walking, Stairs & Daily Activities After Knee Replacement- 22, January 2026
-
 When Knee Pain Needs Medical Attention: Red Flags to Watch
When Knee Pain Needs Medical Attention: Red Flags to Watch- 19, January 2026
-
 Cartilage Damage in Sports: Early Signs Athletes Should Not Ignore
Cartilage Damage in Sports: Early Signs Athletes Should Not Ignore- 15, January 2026
-
 Can You Sit Cross-Legged After Knee Replacement?
Can You Sit Cross-Legged After Knee Replacement?- 13, January 2026
-
 Types of Knee Implants
Types of Knee Implants- 13, January 2026
-
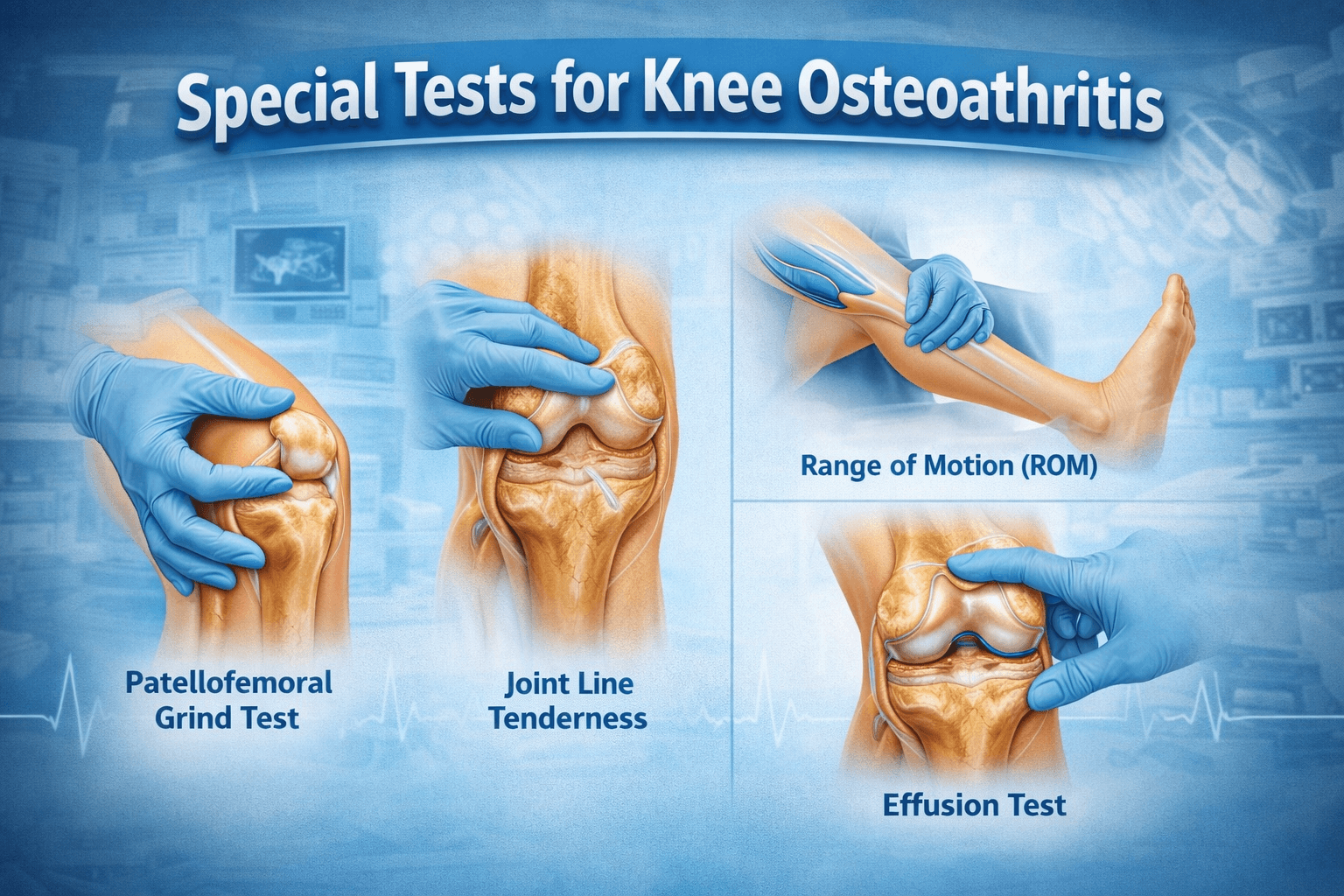
 Special Tests for Knee Osteoarthritis
Special Tests for Knee Osteoarthritis- 7, January 2026
-
 Knee Operation Types: A Comprehensive Guide
Knee Operation Types: A Comprehensive Guide- 7, January 2026
-
 Difference Between Knee Arthritis, Meniscus Tear, and Ligament Injury
Difference Between Knee Arthritis, Meniscus Tear, and Ligament Injury- 30, December 2025
-
 Knee Pain While Walking: When Should You Worry?
Knee Pain While Walking: When Should You Worry?- 30, December 2025
-
 What Happens If Knee Replacement Is Delayed Too Long?
What Happens If Knee Replacement Is Delayed Too Long?- 24, December 2025
-
 How Cartilage Loss Leads to Chronic Knee Pain
How Cartilage Loss Leads to Chronic Knee Pain- 24, December 2025
-
 ACL Tears in Athletes: Symptoms, Treatment Options & Recovery
ACL Tears in Athletes: Symptoms, Treatment Options & Recovery- 19, November 2025
-
 Sports Injuries That Often Lead to Knee Replacement
Sports Injuries That Often Lead to Knee Replacement- 19, November 2025
-
 Orthopedic Care for Elderly Patients — A Complete Guide
Orthopedic Care for Elderly Patients — A Complete Guide- 12, November 2025
-
 How Long Do Knee Implants Last? (10–20 Year Longevity Guide)
How Long Do Knee Implants Last? (10–20 Year Longevity Guide)- 12, November 2025
-
 Importance of Early Diagnosis in Bone and Joint Problems
Importance of Early Diagnosis in Bone and Joint Problems- 28, October 2025
-
 Best Treatment Options for Sports Injuries
Best Treatment Options for Sports Injuries- 28, October 2025
-
 The Difference Between ACL Tear, Sprain, and Rupture
The Difference Between ACL Tear, Sprain, and Rupture- 16, October 2025
-
 Post-ACL Surgery Do’s and Don’ts
Post-ACL Surgery Do’s and Don’ts- 16, October 2025
-
 Early Signs You Might Have an ACL Injury (and When to See a Doctor)
Early Signs You Might Have an ACL Injury (and When to See a Doctor)- 16, October 2025
-
 Does Insurance Cover Robotic Knee Replacement Surgery?
Does Insurance Cover Robotic Knee Replacement Surgery?- 6, October 2025
-
 When Can You Return to Sports After Robotic Knee Replacement?
When Can You Return to Sports After Robotic Knee Replacement?- 6, October 2025
-
 Impact of Obesity on Knee Replacement Surgery and Recovery
Impact of Obesity on Knee Replacement Surgery and Recovery- 30, September 2025
-
 Early vs. Delayed Knee Replacement: Which Is Better?
Early vs. Delayed Knee Replacement: Which Is Better?- 30, September 2025
-
 How Durable Are Knee Implants? A Complete Guide
How Durable Are Knee Implants? A Complete Guide- 24, September 2025
-
 Can You Play Sports After Knee Replacement Surgery?
Can You Play Sports After Knee Replacement Surgery?- 24, September 2025
-
 Key Benefits of Revision Hip Replacement You Should Know
Key Benefits of Revision Hip Replacement You Should Know- 15, September 2025
-
 Revision Hip Replacement vs. Primary Hip Replacement: Key Differences
Revision Hip Replacement vs. Primary Hip Replacement: Key Differences- 15, September 2025
-

-
 Total Knee Replacement Complications: What You Need to Know
Total Knee Replacement Complications: What You Need to Know- 5, September 2025
-
 Can You Play Sports After Hip Replacement Surgery?
Can You Play Sports After Hip Replacement Surgery?- 26, August 2025
-
 Preparing for Knee Replacement: Do’s and Don’ts Before Surgery
Preparing for Knee Replacement: Do’s and Don’ts Before Surgery- 26, August 2025
-

-
 What to Know About Knee Replacement Revision Surgery
What to Know About Knee Replacement Revision Surgery- 18, August 2025
-
 Cost of Hip Replacement in India – What Patients Should Know
Cost of Hip Replacement in India – What Patients Should Know- 11, August 2025
-

-
 Who Is the Best Orthopedic Doctor for Sports Injuries?
Who Is the Best Orthopedic Doctor for Sports Injuries?- 27, July 2025
-
 Success Rate of Robotic Knee Replacement in India
Success Rate of Robotic Knee Replacement in India- 27, July 2025
-
 Why Surgeons Are Switching to Robotic Knee Replacements
Why Surgeons Are Switching to Robotic Knee Replacements- 15, July 2025
-
 Do’s and Don’ts After Knee Replacement Surgery
Do’s and Don’ts After Knee Replacement Surgery- 15, July 2025
-
 Best Robotic Knee Replacement in India
Best Robotic Knee Replacement in India- 7, July 2025
-
 Affordable Robotic Knee Replacement in India
Affordable Robotic Knee Replacement in India- 7, July 2025
-

-

-

-

-

-

-

-
 Orthopedic Meaning, Definition, Types, and More
Orthopedic Meaning, Definition, Types, and More- 6, June 2025
-
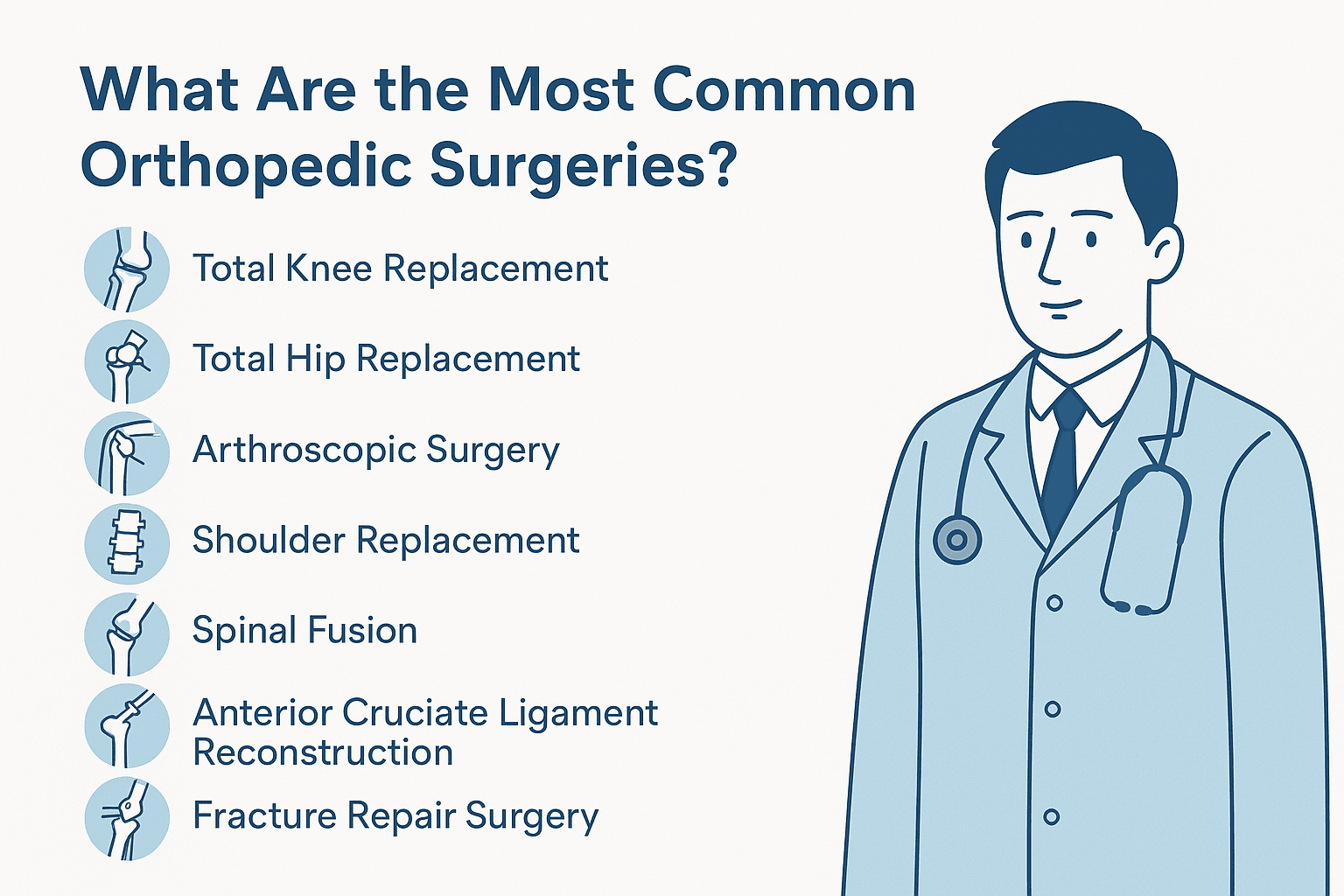
 What Are the Most Common Orthopedic Surgeries?
What Are the Most Common Orthopedic Surgeries?- 24, May 2025
-
 What Does an Orthopedic Doctor Do?
What Does an Orthopedic Doctor Do?- 24, May 2025
-

-

-

-
 Best Orthopedic Doctor for Knee Pain in Faridabad
Best Orthopedic Doctor for Knee Pain in Faridabad- 12, May 2025
-
 How to Prevent Knee Pain with Orthopedic Expert Tips
How to Prevent Knee Pain with Orthopedic Expert Tips- 29, April 2025
-

-
 Best Orthopedic Treatment in Faridabad: What You Should Know
Best Orthopedic Treatment in Faridabad: What You Should Know- 29, April 2025
-

-

-
 Best Knee Replacement Surgeon in Mathura
Best Knee Replacement Surgeon in Mathura- 14, April 2025
-
 Best Knee Replacement Surgeon in Hodal
Best Knee Replacement Surgeon in Hodal- 14, April 2025
-
 Best Knee Replacement Surgeon in Palwal
Best Knee Replacement Surgeon in Palwal- 14, April 2025
-

-

-

-
 Benefits of Minimally Invasive Knee Surgery
Benefits of Minimally Invasive Knee Surgery- 24, March 2025
-
 Best knee Replacement Surgeon in India
Best knee Replacement Surgeon in India- 17, March 2025
-

-
 How to Recover Quickly After Knee Replacement Surgery
How to Recover Quickly After Knee Replacement Surgery- 10, March 2025
-

-

-

-
 Minimally Invasive Arthroplasty: Benefits and Recovery Advantages
Minimally Invasive Arthroplasty: Benefits and Recovery Advantages- 24, February 2025
-
 Common Mistakes to Avoid After Joint Replacement Surgery
Common Mistakes to Avoid After Joint Replacement Surgery- 24, February 2025
-
 Choosing the Right Hip Replacement Surgeon: A Comprehensive Guide
Choosing the Right Hip Replacement Surgeon: A Comprehensive Guide- 17, February 2025
-
 Restoring Mobility: The Role of Knee Replacement Doctors
Restoring Mobility: The Role of Knee Replacement Doctors- 17, February 2025
-
 Orthopedic Trauma Care for Athletes
Orthopedic Trauma Care for Athletes- 6, February 2025
-
 Best Doctor for ACL Tear Treatment
Best Doctor for ACL Tear Treatment- 6, February 2025
-
 Best Sports Medicine Doctor for Knee Injuries
Best Sports Medicine Doctor for Knee Injuries- 6, February 2025
-
 Orthopedic Surgeons: 7 Things You Need to Know
Orthopedic Surgeons: 7 Things You Need to Know- 27, January 2025
-
 Best Joint Replacement Surgeon in Greater Faridabad
Best Joint Replacement Surgeon in Greater Faridabad- 27, January 2025
-
 Best Knee Replacement Surgeon in Palwal
Best Knee Replacement Surgeon in Palwal- 20, January 2025
-
 Best Knee Replacement Surgeon in South Delhi
Best Knee Replacement Surgeon in South Delhi- 20, January 2025
-
 Signs You May Need a Knee Replacement: Insights from a Surgeon
Signs You May Need a Knee Replacement: Insights from a Surgeon- 13, January 2025
-
 Restoring Mobility: The Role of Knee Replacement Doctor
Restoring Mobility: The Role of Knee Replacement Doctor- 13, January 2025
-
 Robotic Knee Replacement Surgery in Delhi
Robotic Knee Replacement Surgery in Delhi- 30, December 2024
-
 Robotic Orthopedic Surgery: Revolutionizing Joint Replacement and Repair
Robotic Orthopedic Surgery: Revolutionizing Joint Replacement and Repair- 30, December 2024
-
 Robotic Knee Replacement vs. Traditional Surgery: A Comparative Guide
Robotic Knee Replacement vs. Traditional Surgery: A Comparative Guide- 23, December 2024
-
 How to Make Joints Stronger: A Comprehensive Guide
How to Make Joints Stronger: A Comprehensive Guide- 23, December 2024
-
 Common Knee Conditions and How a Knee Surgeon Can Help
Common Knee Conditions and How a Knee Surgeon Can Help- 16, December 2024
-

-

-
 Orthopedic Surgeons: 7 Things You Need to Know
Orthopedic Surgeons: 7 Things You Need to Know- 6, December 2024
-
 Top 5 Mistakes After Knee Replacement
Top 5 Mistakes After Knee Replacement- 25, November 2024
-
 Advantages and Disadvantages of Robotic Knee Replacement
Advantages and Disadvantages of Robotic Knee Replacement- 25, November 2024
-
 When to See an Orthopedic Specialist: Recognizing Early Signs
When to See an Orthopedic Specialist: Recognizing Early Signs- 15, November 2024
-
 Benefits of Robotic-Assisted Knee Replacement Surgery
Benefits of Robotic-Assisted Knee Replacement Surgery- 15, November 2024
-
 Knee Replacement Surgery Cost
Knee Replacement Surgery Cost- 8, November 2024
-
 Best Robotic Knee Replacement Surgeon in Faridabad
Best Robotic Knee Replacement Surgeon in Faridabad- 8, November 2024
-

-
 Knee Replacement Surgery: Types, Benefits, and Recovery Timeline
Knee Replacement Surgery: Types, Benefits, and Recovery Timeline- 28, October 2024
-
 What is Osteoporosis? Symptoms, Causes, and Prevention
What is Osteoporosis? Symptoms, Causes, and Prevention- 21, October 2024
-
 Signs It’s Time for a Knee Replacement: When to Consult a Surgeon
Signs It’s Time for a Knee Replacement: When to Consult a Surgeon- 18, October 2024
-
 Understanding Different Types of Arthritis: Symptoms and Causes
Understanding Different Types of Arthritis: Symptoms and Causes- 11, October 2024
-
 Taking Care After Knee Replacement Surgery
Taking Care After Knee Replacement Surgery- 15, December 2022
-
 Amazing Ways to Get Relief from Arthritis Pain Naturally
Amazing Ways to Get Relief from Arthritis Pain Naturally- 2, December 2022
-

-
 How Does Fat Affect Arthritis?
How Does Fat Affect Arthritis?- 4, November 2022