
Primary and Revision Total Hip Replacement Surgery
Arthritis in hip joint can lead to difficulty in walking and performing daily chores of life. Primary arthritis of Hip joint is uncommon in Asian, Hispanic or Black populations. Mostly, patients in these ethnicities suffer with secondary arthritis due to trauma, dysplasia of hip, avascular necrosis, inflammatory arthritis or infection in the hip joint. Due to the secondary nature of the disease, they appear at an earlier age, maybe as early as the second decade of their life. This early onset poses increased morbidity for the patient and surgical challenges for the orthopaedic surgeon. The inability to perform normal activities at young age produces feelings of hopelessness in patient and worsens physical and financial output. Due to lack of awareness and at times remote access to the healthcare system causes further delays in seeking medical advice from an orthopaedic surgeon.
Patients with hip arthritis present with pain around their hip joint and difficulty in walking. They also have difficulty in sitting on the floor or squatting. Few patients present with complaints of not able to perform marital obligations. Detail history is taken to ascertain the underlying cause. Proper examination is performed to assess movements in the affected hip joint. Radiological and blood investigations are performed as per the requirements. MRI and CT scan (with 3D reconstruction) provided the detailed anatomical extent of disease and any associated loss of bony architecture. It is important to get as much information as possible before planning treatment options.
Patients presenting in early stage of the disease are given course of analgesics and physiotherapy to the hip joint. They are also advised to go cycling or swimming. These measures help in strengthening hip muscles and keeping the joint mobile. Patients with advanced disease have minimal movement in their hip joints hence they should opt for surgical options for their underlying arthritis.
Total hip replacement surgery, since its inception in 1960 has been a reliable and proven technique for underlying arthritis. It has been called “Operation of the century” as it helped improve lives of patient suffering with debilitating arthritis. There has been continuous improvement in design and material of acetabular & femoral components and the method of fixation to the host bone. The success rate for total hip replacement has improved from approx 77% survivorship for Charnley’s arthroplasty to almost 92-100% for modern-day implants. Over the last 4-5 decades, total hip replacement surgery has gradually improved outcome and patient satisfaction. Continuous advancement in metallurgy and bearing technology has made this success possible. Improvement in surgical technique and advancement in the field of anesthesia has improved pain management and post-op rehabilitation in these patients.
Total Hip Replacement implants mainly fall into two categories – cemented and uncemented. In cemented implants, antibiotic-laden polymethyl-methacrylate is used to fix the implant to the bone. In an uncemented implant, it directly fixes to the bone. Uncemented implants have a larger global acceptance today. Another major advancement occurred in the “bearing surface” between the acetabular and femoral implant. This is the surface on which hip joint moves after the surgery. Sir John Charlney introduced high-density polyethylene as bearing surface and it revolutionized the replacement surgery. Later, the metal-on-metal bearing was introduced in 1960s. Failure rates were higher than acceptable with these two bearing surfaces. Presently used bearings are highly crossed-linked polyethylene with cobalt chrome metal, highly crossed-linked polyethylene with delta ceramic and delta ceramic on delta ceramic. All three have proven past record and used worldwide. There is a general consensus to use Ceramic on Ceramic in younger patients and in those older patients who are physically active.
Complex Total Hip Replacement
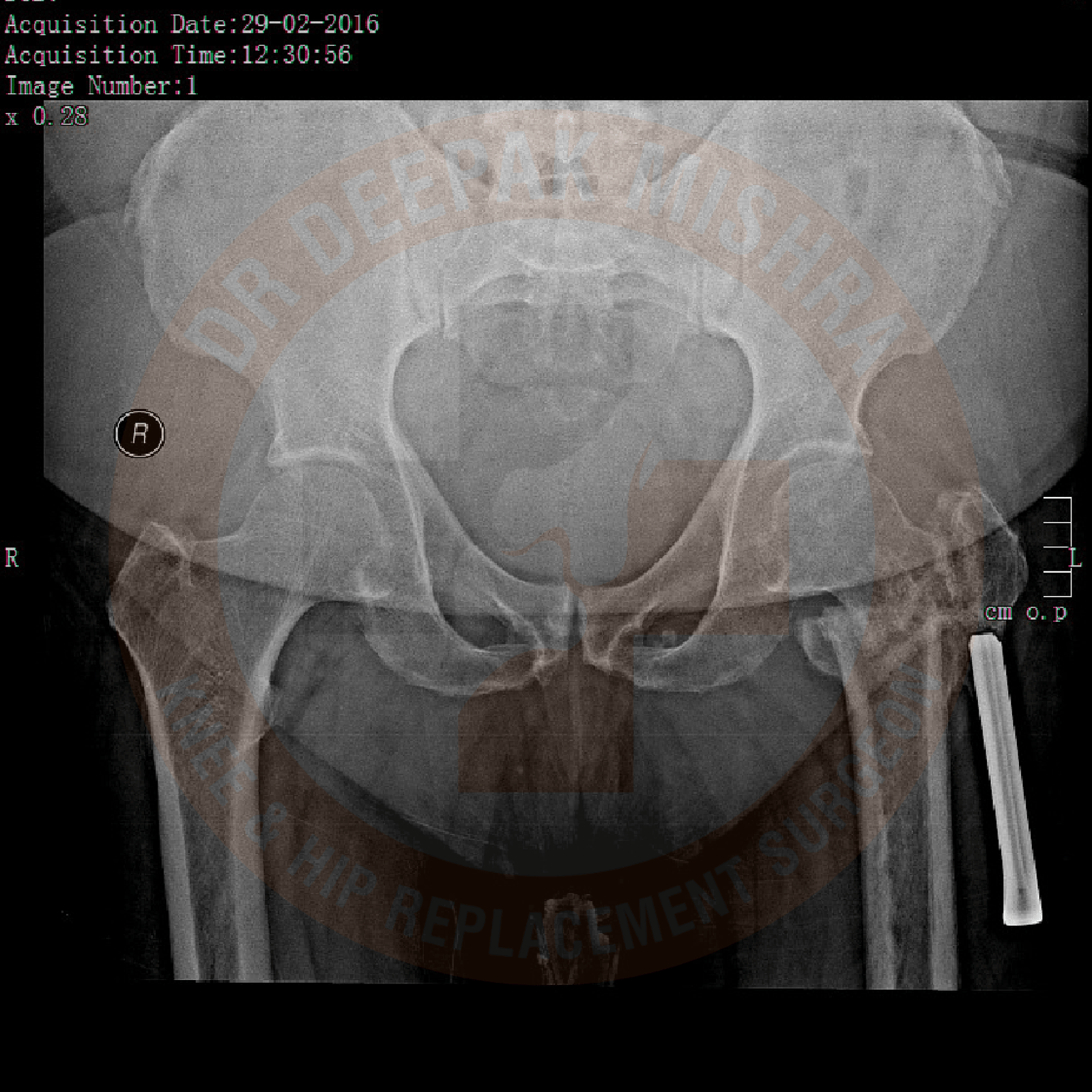
Pre Operative
Post Operative
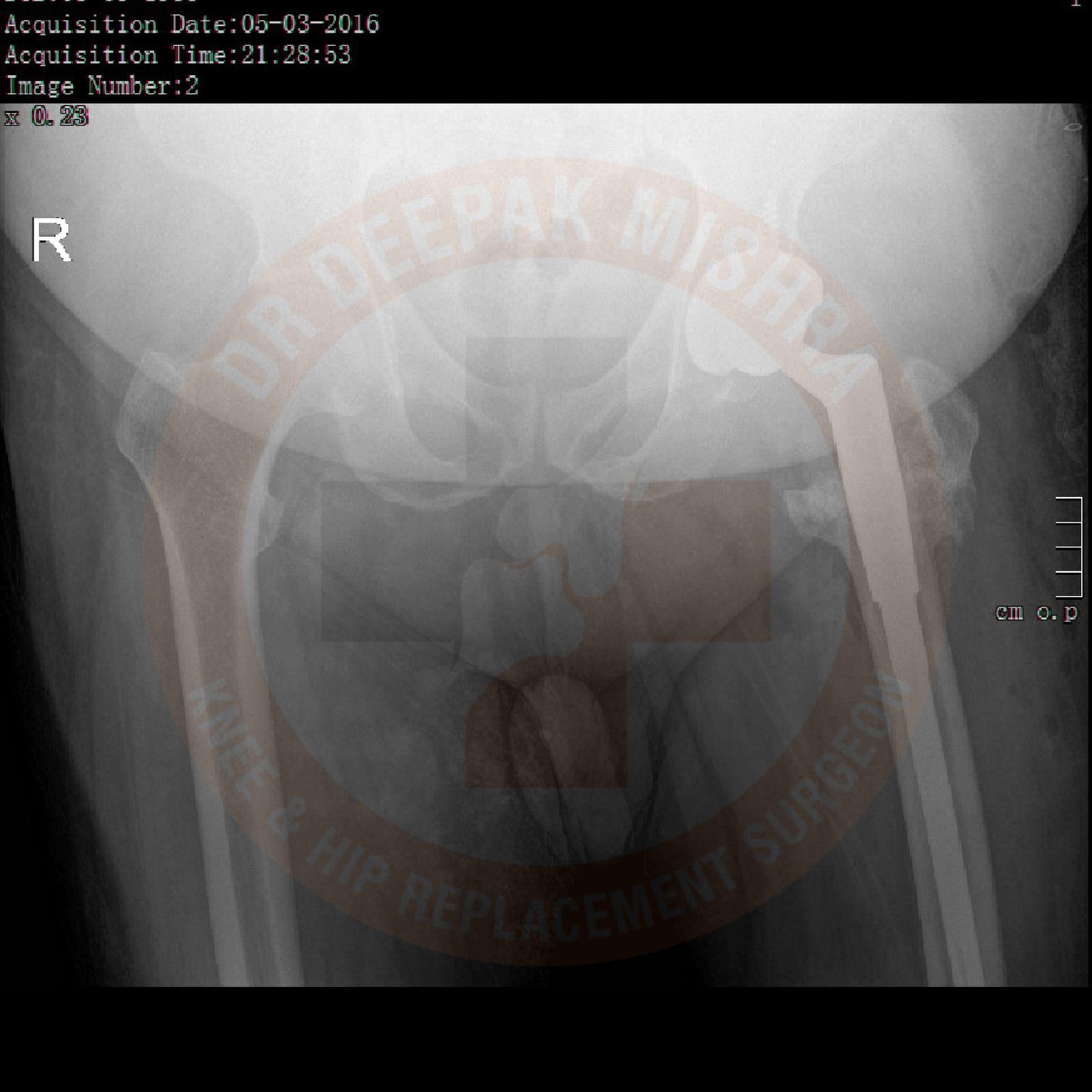
Revision Total Hip Replacement
Pre Operative

Post Operative
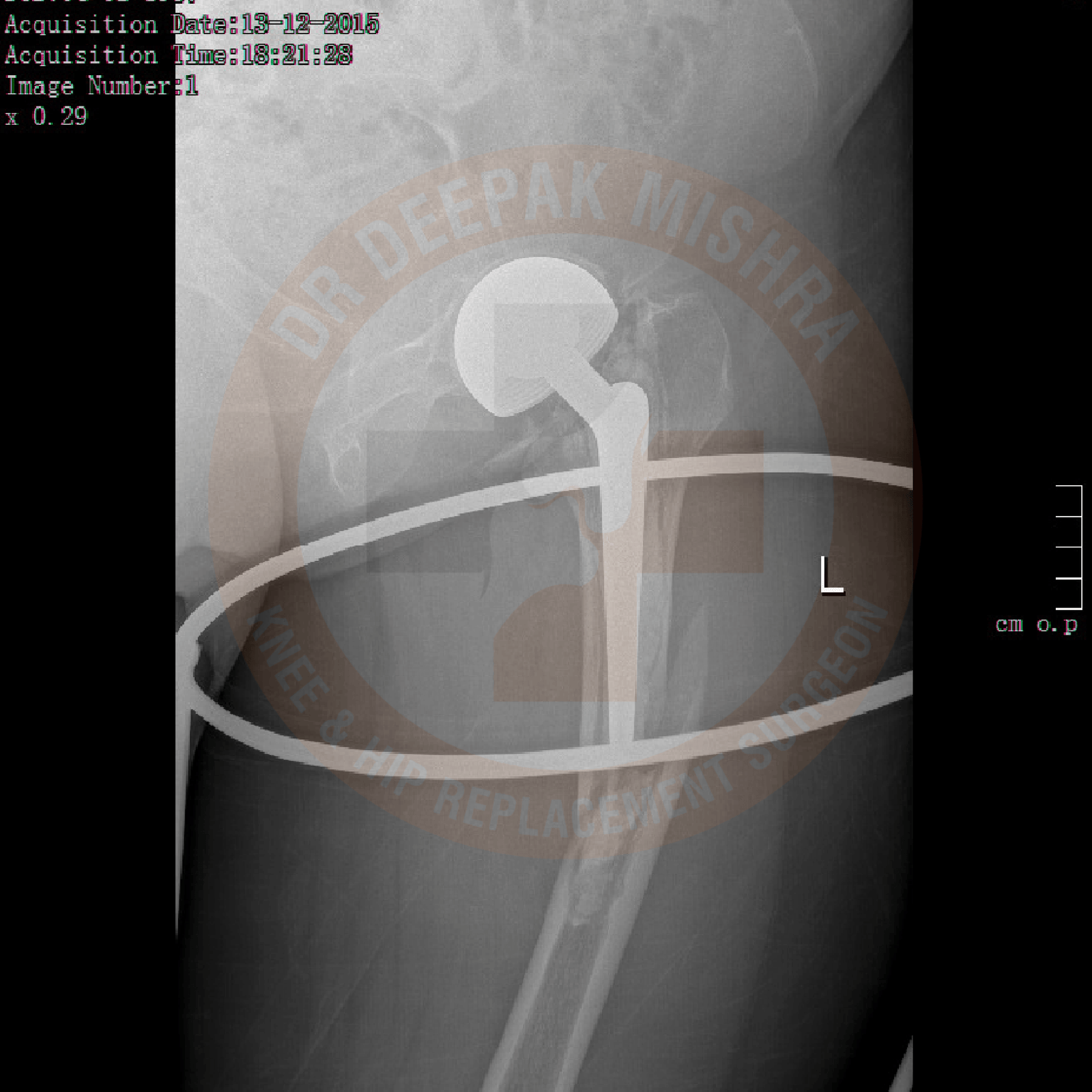
Revision Total Hip Replacement

Pre Operative
Post Operative
Total Hip Replacement
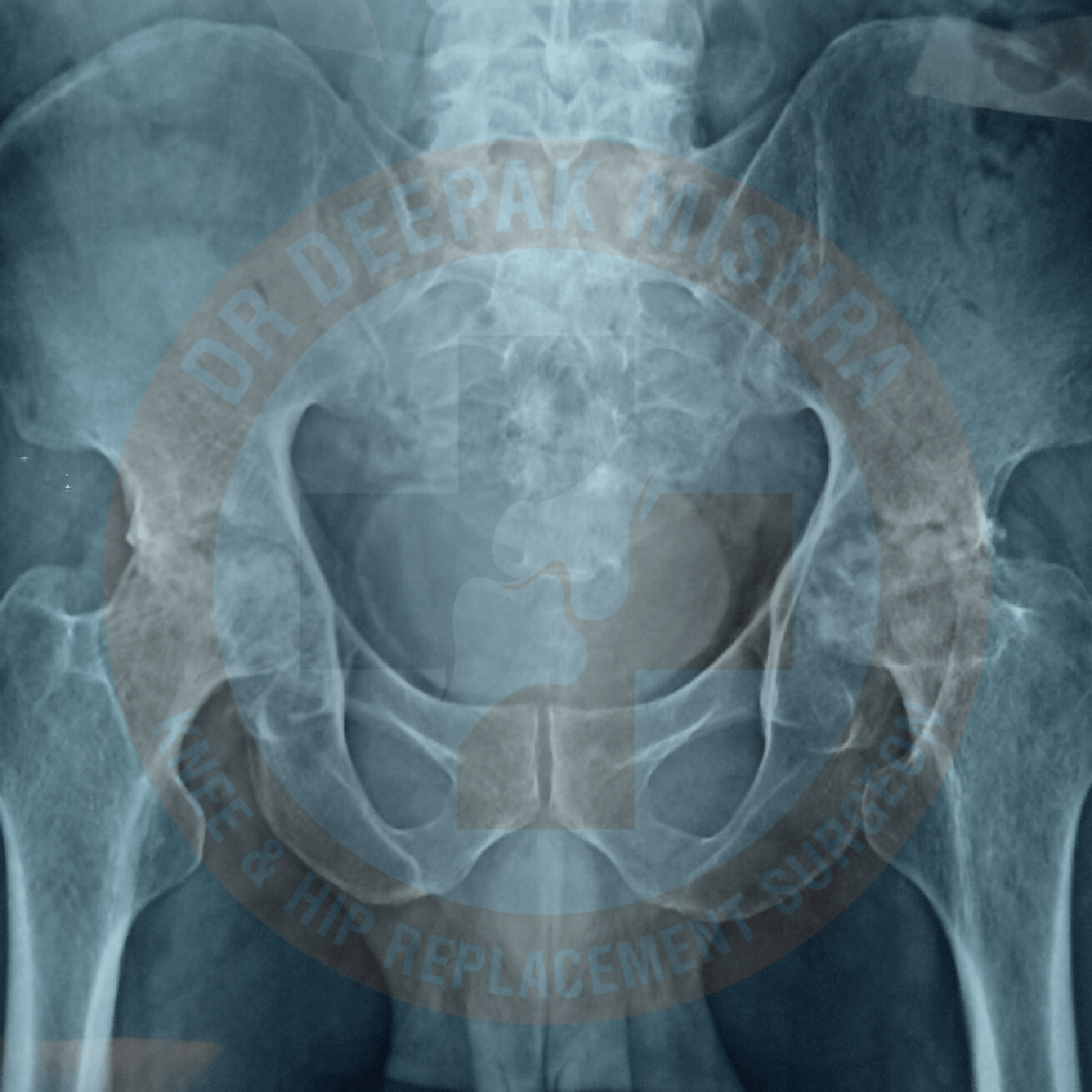
Pre Operative

Post Operative
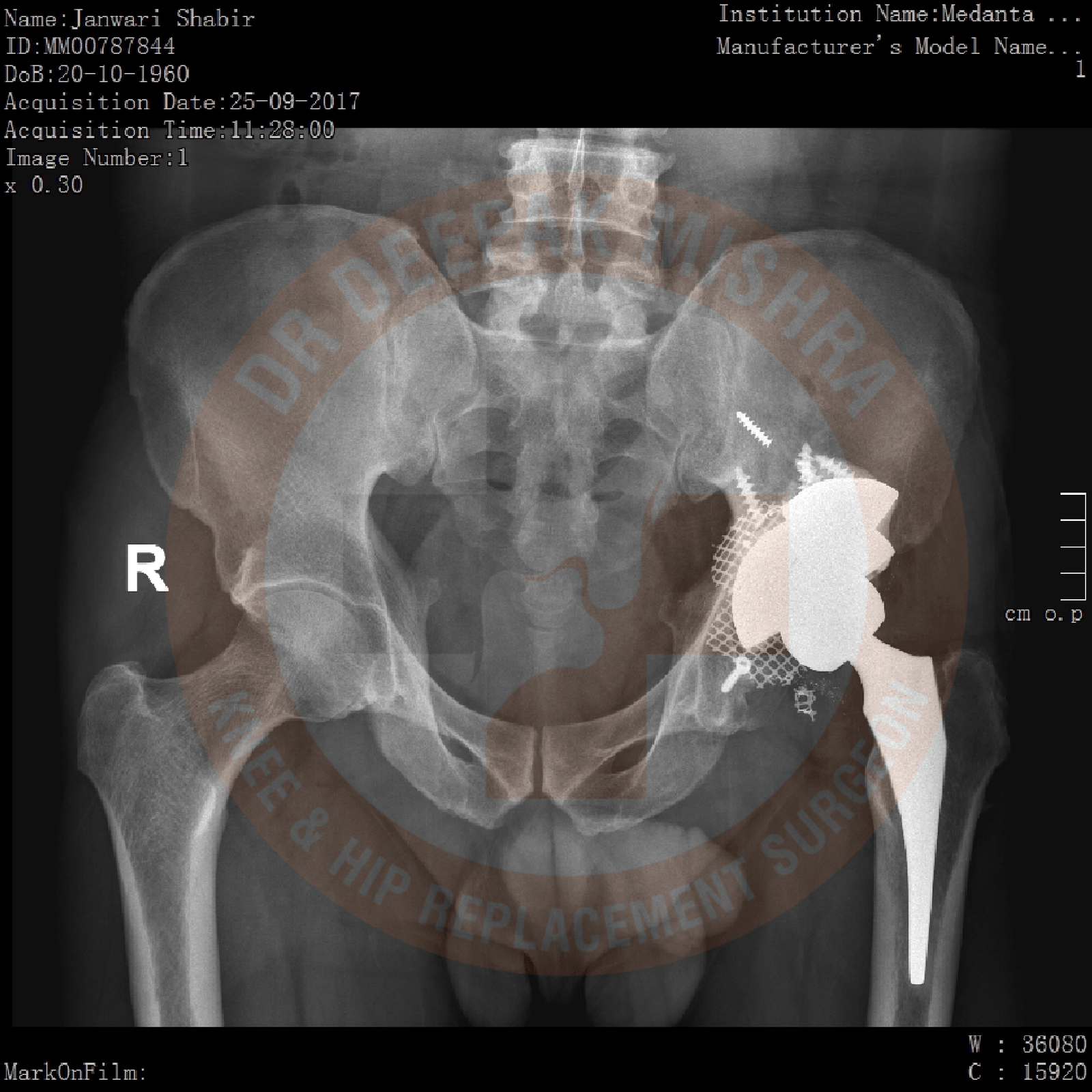
Total Hip Replacement Fused Hip Joint

Pre Operative
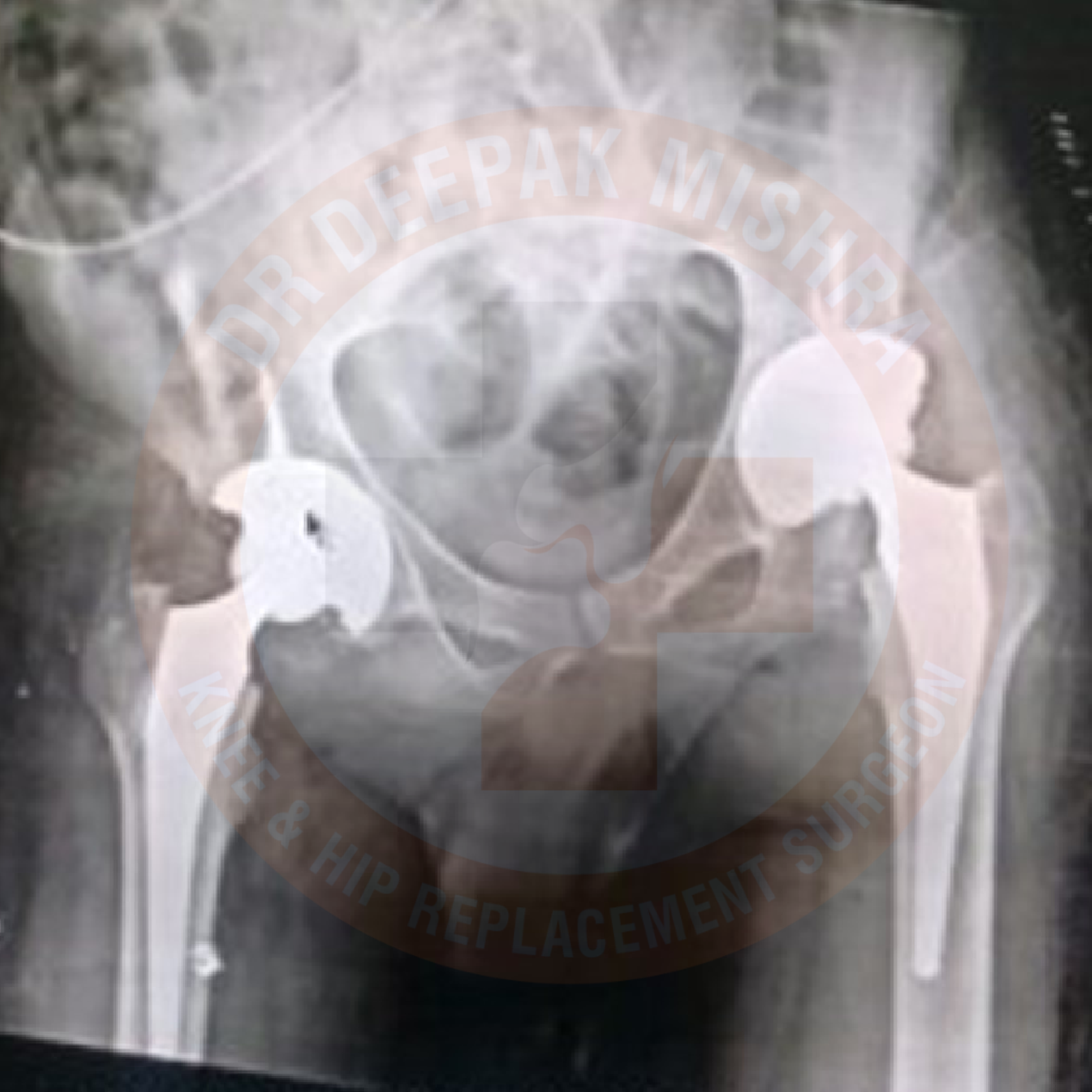
Post Operative
FAQ about Total Hip Replacement Surgery:
What is the cause for Hip joint arthritis in young patients?
It usually occurs due to trauma to the hip joint, avascular necrosis (lack of blood supply to ball of the femur), infections (tuberculosis/septic), childhood hip problems (congenital hip dislocation, Perthe’s disease, slipped capital femoral epiphysis, etc) and inflammatory arthritis like rheumatoid arthritis or ankylosing spondylitis.
What problem a hip arthritis can give to the patients?
Due to damaged hip, patients experience pain in day-to-day activities. They have difficulty in sitting crossed leg, squatting or using stairs. As disease progresses with time, the deformities appear in hip joint leading to reduced mobility and subsequently these patients become bedridden. Increasing deformity also produces changes in spine and knee joints, if not treated on time. Few patients presents with complaints of not able to perform marital obligations.
How is hip arthritis diagnosed?
Your doctor will do clinical examination of hip joint, spine and other joints of your body. Radiological examination (X-rays and MRI) and blood investigations will be performed based on clinical findings. It varies from patient to patient as per their underlying problem.
What is Total Hip Replacement surgery?
In total hip replacement surgery, we remove the damaged femoral head (ball) and cartilage of the acetabulum (cup) and replace it with metal implants. During the surgery, size of the acetabulum and femoral head are measured to provide optimized size of the implant.
Is this surgery successful in young patients?
Yes, it is very successful. The more and more young population is undergoing Total Hip Replacement surgery across globe now-a-days. This has been made possible due to –
(a) better surgical technique
(b) advancement in implant design
(c) improvement in metal quality
(d) improvement in ball-socket material (e.g, ceramic)
When should one undergo Total Hip Replacement surgery?
Patients should seek surgery when their hip pain limits day-to-day activities, hip pain interferes with their sleep, no relief with any medications or deformity appears to set in.
How is surgical period planned after admission?
You will be admitted one day before surgery. You would already have seen anesthesia team with your routine reports so that you get fitness for surgery. Your anesthetist will make you numb at your operating area. You will remain awake throughout the procedure. You can listen to songs if you wish to. The surgeon will perform surgery as per the protocol and insert new hip joint which fits best in your joint. Once you are transferred to recovery room, you will be started on oral diet.
When can I start walking after Total Hip Replacement?
You can start to walk with help of walker once the effect of anesthesia wears out completely, that can happen on same day evening or next day morning depending on the time of your surgery. Physiotherapist will help you in walking and teach you few exercises.
When do patients get discharged from hospital?
Once you have completed the “post-operative pathway” as per the hip replacement surgery protocol, you are fit to go home. It can vary from 2-4 days after surgery.
Do I need to take any special care after surgery?
Yes, you should be very careful and protect your new hip joint so that it lasts long with you. You should avoid – sitting crossed leg, sitting on floor, squatting, high-impact activities and bending forward. It may cause damage to ball & socket or may cause ball popping out of your socket.
